Schools and COVID-19: Frequently Asked Questions from Parents and Caregivers
NOTE: As of May 15th, 2021, the modules will no longer be updated. We invite you to visit the CDC’s website to find the most up-to-date information related to school re-openings, mitigation strategies, testing, screening, monitoring, and guidance on how to safely return to school in person.
Do you have questions about schools and COVID-19? We’ve assembled answers to many frequently asked questions below.
For detailed information about strategies schools may use to reduce COVID-19 risk, see our educational modules for schools and districts here.
Planning for in-person school return
How do I know if in-person school is right for my child or our family?
- Every family should make the decision about returning to in-person schooling that is right for them.
- Children with compromised immune systems and some health conditions that put them at higher risk of severe illness may want to learn from home if that option is available; some may need specific kinds of protective equipment for in-person learning. Talk to your child’s doctor to see what’s best for your child. If a member of your household is high risk (because of a compromised immune system or health condition) they should discuss whether in-person school is the right choice with their healthcare provider.
Why are some schools bringing back younger kids before older kids?
- There are several reasons why schools have made the decision to reopen with younger students first. Some students have continued to have trouble with virtual learning, particularly special needs students. Others have not had consistent access to technology to participate in virtual learning. Learning loss in younger students may be greater and longer lasting.
- Also, children of any age can be infected with COVID-19 and spread the virus to others, but the likelihood they will be infected, and the seriousness of the illness seem to be lower in kids ages 10 and younger. Young children may also be less likely to spread the disease to others if they get infected. That’s why some schools are focusing on younger learners first for in-person school; the risk of viral spread may be lower in this group.
What types of risk reduction measures are being used to keep kids safe in schools?
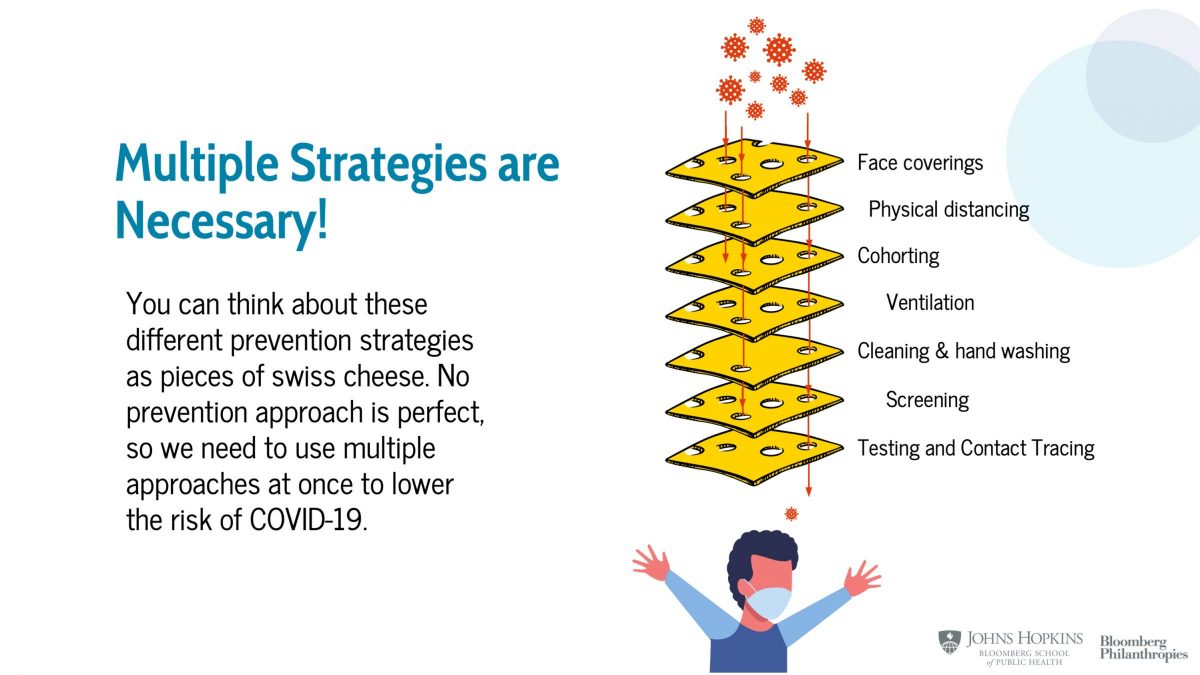
- Your school may be using a combination of strategies to help keep kids safe in school including reducing the number of students in the building at one time to allow for more distancing, requiring masks, providing personal protective equipment for staff and students, reducing mixing between different groups of students, improving ventilation, screening students for symptoms of COVID-19, cleaning, testing for COVID-19, and contact tracing.
- More strategies are better. Why? No one strategy is perfect. When we use many strategies, we reduce the chance that if any of strategy fails, COVID-19 will spread.
Why is my school using a hybrid schedule? What is a hybrid schedule?
- “Hybrid” just means a combination of two different things. In the case of schools, it’s a combination of in-person and remote learning. By having some students learn remotely some of the time, schools can reduce the number of students in schools at any one time, allowing more space between desks and in the halls. Students may trade off days or part-days between remote and in-person learning.
When should my child stay home from school?
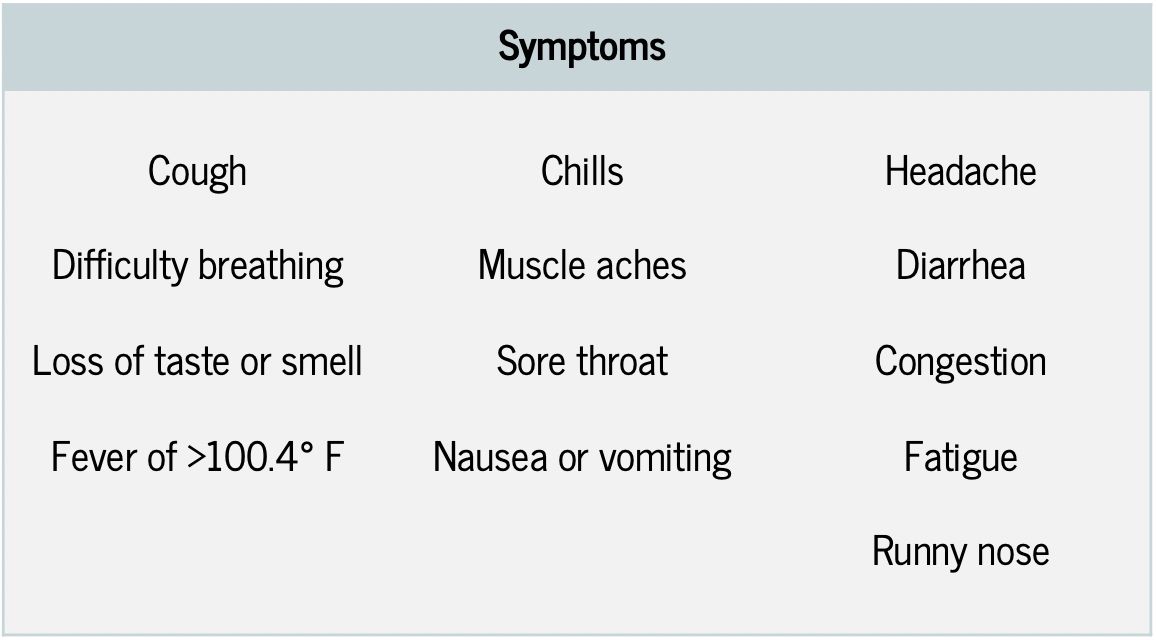
- Your child should stay home from school if they have any symptoms of COVID-19. COVID-19 symptoms include cough, shortness of breath, difficulty breathing, loss of taste or smell, fever >100.4 degrees F, chills, muscle aches, sore throat, nausea or vomiting, headache, diarrhea, congestion, fatigue, and runny nose.
- Call your pediatrician to determine if your child needs to be seen and/or have a COVID-19 test.
- Talk to your child’s school about local guidance for when your child can return to school after they are feeling better.
What specific indicators might my school be monitoring to inform decisions about whether to open or close?
- Schools will be monitoring COVID-19 both inside and outside the building to inform their decisions about when to open or close. Two numbers are often used to talk about how much COVID-19 is in the community:
- New case rate is the average number of new cases per day for every 100,000 people in a given time period. The CDC uses 7 days.
- The test positivity rate, which is the percent of all COVID-19 tests that are positive in a certain time period. Remember, this only tells you about people who got a test, so it’s not necessarily the percent of people in your community with COVID-19, since many people don’t get tested.
- Schools may also look for clues about COVID-19 inside of schools by monitoring the number of students and staff who are absent, the number of people who say yes to COVID-19 screening questions, and the number of people at the school who are in quarantine or self-isolation.
Where can I find out what my school or district’s plans are?
- Ask your school principal where to find these plans. Many school districts have posted their guidelines and plans on their websites. Your school may have additional details about how the plan will work in your child’s school, specifically.
What does my child need to bring to school?
- Make sure your child has a mask for school and send an extra in case it gets wet or dirty. (Label them clearly!)
- Send an extra layer if your child’s classrooms will have windows open.
- Find out if your child will have water available or if you need to pack a water bottle from home.
- Find out if your child will go outside no matter what the weather for recess and send the right clothes for this.
How can I plan for returning to in-person school?
Download Back To School Handout (pdf)
- The CDC has a helpful checklist here. It includes making a plan to:
- Check your child for signs of illness every morning before school. Remember that if your child has had close contact with someone who has COVID-19, they should not go to school.
- Find out the person at school to contact if your child gets sick.
- Explain the importance of maintaining distance, wearing a mask, washing hands, and avoiding sharing food, water bottles, or devices at school.
- Make sure your contact information is up to date so the school can reach you during the day.
What happens during the school day?
My school is using cohorts. What’s a cohort?
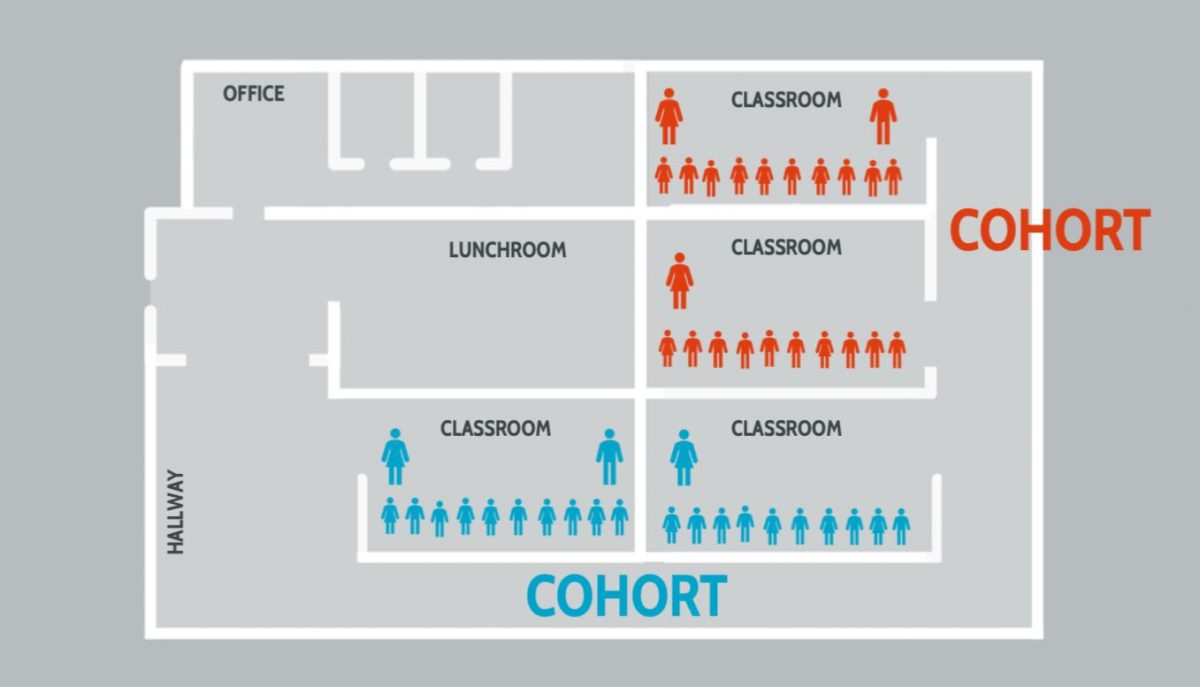
- Cohorts are small groups of students and staff who work, learn and eat together. Their contacts are limited to the people in their cohort, and they do not have in-person interaction with others in the school building. People who are in a cohort together should still mask and physically distance from others in their cohort.
- One simple example of a cohort might be two second grade classrooms (10 students each), their teachers (2 adults), and an instructional aide who supports both classrooms.
- Schools use cohorts to limit the number of people your child comes into contact within any given day. This helps to decrease the chance that they come into contact with someone who has COVID-19. If someone in the school becomes sick, the school can quickly quarantine the cohort while they work to determine whether the sick person has COVID-19. If it is COVID-19, the school may be able to close just that cohort instead of a whole grade or the entire school.
What about lunch, bathroom, PE and recess?
- Mealtimes can pose a safety risk because students take off their masks. There are also times when students usually mix with kids and adults outside their class. Special attention should be given to physical distance and ventilation during eating. To keep cohorts together, students may eat in classrooms. Contact with food does not seem to be a major way that COVID spreads. However, boxed or packaged foods may be used to avoid multiple people handling student meals. Good hand hygiene before, during, and after eating is important.
- Recess is important for children’s physical health and for their learning. Ventilation is better outdoors, so the risk of spreading COVID is lower. Recess should be outdoors whenever possible. It is important to stick to cohorts, masking, and distancing, even outside.
- Physical education classes should also be outside when possible, following the recess guidance above. Masks, distancing, and cohorts should be maintained in PE. Some schools may choose to have the PE teacher provide instruction virtually to avoid mixing cohorts.
- Regular cleaning and supplies for proper hand washing are needed in school bathrooms. It is important to avoid crowding in bathrooms. Schools should limit the number of people who are able to use a bathroom at one time based on the size of the space.
What about after-school sports and activities?
- After-school sports and other activities can make it difficult to prevent mixing of students in different cohorts. The American Academy of Pediatrics suggests modifying youth sports to reduce infection risk. These changes include focusing on non-contact activities such as practice drills where social distance can be maintained, screening athletes and coaches for COVID-19 symptoms and exposures, small group training, hand washing stations, and limiting spectators. Athletes should be encouraged to wear cloth face masks during outdoor training, competitions, and on the sidelines. Outdoor sports carry less risk than indoor sports and face coverings are strongly recommended for all athletes* competing indoors in addition to other mitigation strategies. (Note: Face coverings during competition are not recommended for athletes competing in the water, competitive cheerleaders, gymnasts, or wrestlers due to choking hazards and/or potential for blocked vision).
How can transportation to and from school be made safer?
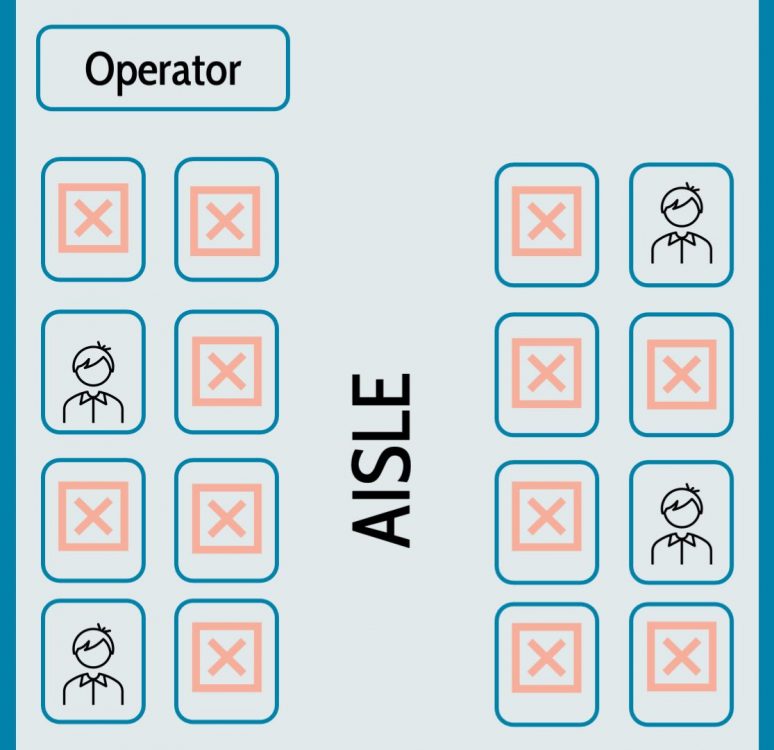
- The same strategies we use to prevent transmission in school can be used for transportation to and from school. This means practices of masking, physical distancing, cohorting, ventilation, and cleaning should be followed on school buses, too. All riders should wear masks, buses should include hand sanitizer dispensers, only one student should sit in each row (except for students in the same household), windows should be kept open to increase ventilation when the weather allows, and all bus surfaces should be cleaned regularly.
- If students ride public transit, choosing the least crowded areas, wearing a mask, keeping distance from others, and using hand sanitizer can help reduce the risk of transmission.
- If students walk or bike to school, encourage masking and maintaining distance between people as they walk.
How might classrooms be different during COVID-19?
- Your child’s classroom might be set up differently. First, there may be fewer desks and fewer students to allow for more distance. Some shared materials may have been put away.
- Some schools may use clear plexiglass shields or screens around some desks or tables.
- Desks may be set up so they are all facing in one direction rather than in a circle or square.
- Windows may be open, if it’s safe to do so.
- You may see a portable air purifier if there is not enough ventilation in the room.
- You may see hand sanitizer dispensers or portable sinks.
- Water fountains may be turned off to prevent spreading illness.
Masks and face coverings
Why does my child need to wear a mask or face covering?
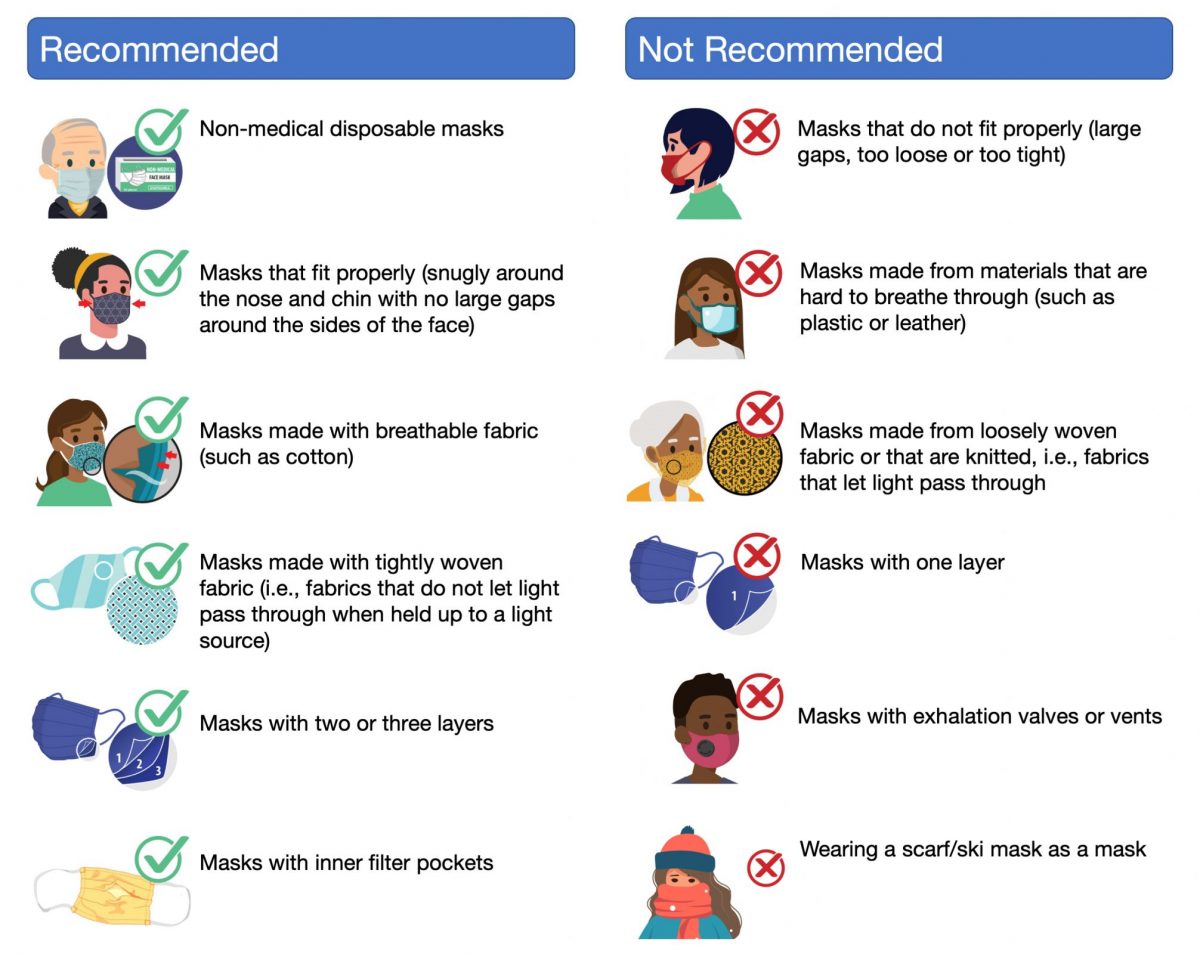
- Masks can be very effective at preventing transmission of COVID-19, but they’re most effective when everyone is wearing them. Cloth or surgical masks protect others from the wearer’s droplets, so if everyone is wearing them, everyone has protection. Different masks offer different levels of protection for your kids, so it’s important to identify which masks are suitable for school: cloth and surgical (not neck gaiters, masks with expiration valves, or face shields alone).
What kind of mask should I get for my child? Do they need a mask and face shield?
- Different masks offer different levels of protection. Cloth and surgical masks are recommended for school. Face shields alone are not an adequate substitute for a mask, but they can be used with a mask. However, research has not yet confirmed that using a shield with a mask offers more protection than just wearing a mask. Neck gaiters and masks with expiration valves are not as effective as cloth and surgical masks and should not be used for school.
Should my child wear two masks?
- More layers provide more protection when it comes to masks. There are a few options for getting more layers. First, you can use a cloth mask that has multiple layers of fabric. Second, some masks have built in filter pockets. You can buy filters to put in the pockets to create extra layers. Third, you can wear two masks- a disposable surgical mask underneath a cloth mask. The cloth mask should push the surgical mask against the face. Whatever you choose, make sure that the mask fits well and that your child can see well and breathe easily.
Are there specific masks for students and staff who are deaf, hard of hearing or who receive speech therapy?
- For students who lip read or those who need to see other people’s facial expressions or the way their mouths move when they make sounds (for example, for speech therapy), special masks with clear mouth panels are available. Some schools may have these available for staff and students. They are also available for purchase.
What if my child has trouble wearing a mask?
- Most children ages 2 and older can wear a mask although there are some health and developmental conditions that prevent people from wearing masks. What can you do if your child has trouble wearing their mask consistently? Here are some tips:
- Find a mask that fits. Look for child-sized masks for small faces. A mask that fits well is less likely to be irritating.
- If possible, let your child help choose the mask or let them personalize it with fabric markers. When kids like their masks, they’re more likely to wear them.
- Model mask wearing. If everyone else in your household wears a mask, your child is more likely to do so.
- For young children, talking about the benefits of masks and how they can help others may be helpful. Young children love to feel helpful. Explain that when we wear masks, we’re like superheroes, we help protect other people.
Screening and testing
What kinds of COVID-19 screening are schools doing? Why?
- Screening programs are designed to find students who have symptoms of COVID-19 or have been exposed to COVID to prevent them from exposing others. Screening can be done in many ways. Some schools ask families to answer a series of questions before they come to school using an app. Other schools may ask students these questions in person and may check students’ temperatures as they arrive at school. It’s important to know that many people who have COVID-19 do not have symptoms and people who don’t have symptoms can still spread the virus to others. So, screening alone won’t prevent students with COVID-19 from coming to school.
Is one screening process better than another?
- No. There is no strong evidence in favor of one screening process over another. Screening must be part of a larger effort that includes face coverings, distancing, ventilation, and other strategies.
What do I do if my child is feeling sick and I’m not sure if it’s COVID-19?
- If your child is feeling sick, you should not send them to school or other activities. Call your pediatrician if you’re not sure your child needs to be seen and/or have a COVID-19 test. Be sure to follow your school’s procedure to inform them that your child is sick.
What kind of COVID-19 test does my child need if I think they might have COVID-19 or they have been exposed?
- Two types of tests are used to diagnose COVID-19.
- Molecular Test (also known as a “PCR test”)
- What is it? A molecular test detects the genetic material of the COVID-19 virus
- How is the sample taken? Nose swab, throat swab, or saliva
- How long does it take to get results? Same day to a week or more depending on the testing location
- What does it show? If someone has COVID-19 infection at the time of the test
- What does it NOT do? Determine if someone was infected with COVID-19 in the past
- Antigen Test
- What is it? An antigen test detects proteins on the surface of the COVID-19 virus
- How is the sample taken? Nose swab, throat swab
- How long does it take to get results? 15 min to 1 hour
- What does it show? If someone has COVID-19 infection at the time of the test
- What does it NOT do? Not FDA approved to test people without symptoms. Test results are less accurate than molecular tests.
- Molecular Test (also known as a “PCR test”)
- Some schools may accept either a molecular or antigen test and others may only accept a negative molecular test result.
- Note that Antibody Tests are NOT used to diagnose COVID-19. These tests check the blood for antibodies against COVID-19 virus. Antibody tests can show if someone has been infected with COVID-19 in the past.
How long should I wait to test my child for COVID-19 after they are exposed to the virus?
- After someone is exposed to COVID-19, it takes a little while for levels of the virus to get high enough in the body for a test result to come back positive. Most people who have the virus will test positive about 5-6 days after they are exposed, but it could take as long as 14 days in some people. You should get a test 5 or more days after exposure. It’s important to quarantine based on local public health guidance (usually 14 days after exposure) to avoid spreading the virus.
My school is offering testing for students with no symptoms and those who have not been exposed to anyone with COVID-19. Why?
- Schools may test students and/or staff with no symptoms and no exposures. This testing approach is called “surveillance testing.” This testing approach will help to identify how much COVID-19 there is in the school that may be going undetected. This can help schools catch cases in people who don’t have symptoms. Schools can use the information to help make decisions about opening and closing. Schools may test all children and staff at one time or a small percentage on a regular basis. They could also do one-time testing of everyone at a specific timepoint, for example when a school reopens that was closed.
My school is offering "pooled" COVID-19 testing. What is this?
- “Pooled” testing is a specific way to test people for COVID-19 in groups.This approach reduces cost and burden on labs. Samples from multiple people are taken just as they are for individual testing. After they are collected, the samples are combined into one pool and tested as a mixture. If the pooled test comes back negative, all of the people are assumed to be negative. If the pool comes back positive, we know that one or more people is positive, but we don’t know who is positive. The next step, then, is for everyone in the pool to get an individual COVID-19 test.
What if there is an infection at school?
If my child or someone in their class has COVID-19 what might happen?
- If your child tests positive for COVID-19, the local health department will be notified. They will notify you and the school. They can and must notify your child’s close contacts that they have been exposed to someone with COVID-19. This is so those contacts can quarantine, monitor for symptoms, and get tested. For example, your child’s school might send a message to your child’s cohort stating that someone in the cohort tested positive for COVID-19 and that the entire cohort will be quarantined. The school cannot share your child’s name or information with anyone without your permission.
What is contact tracing?
- Contract tracing is a way to interrupt the spread of disease from person to person in communities. It is a public health measure to let people know they’ve been exposed to COVID-19 and need to monitor for their symptoms, self-isolate, and be tested. When a student or staff member tests positive for the virus, the local public health department and/or school determines who the student has been in contact with using contact tracing. This is important because people who have been exposed to the virus but don’t have symptoms could spread the virus without knowing it.
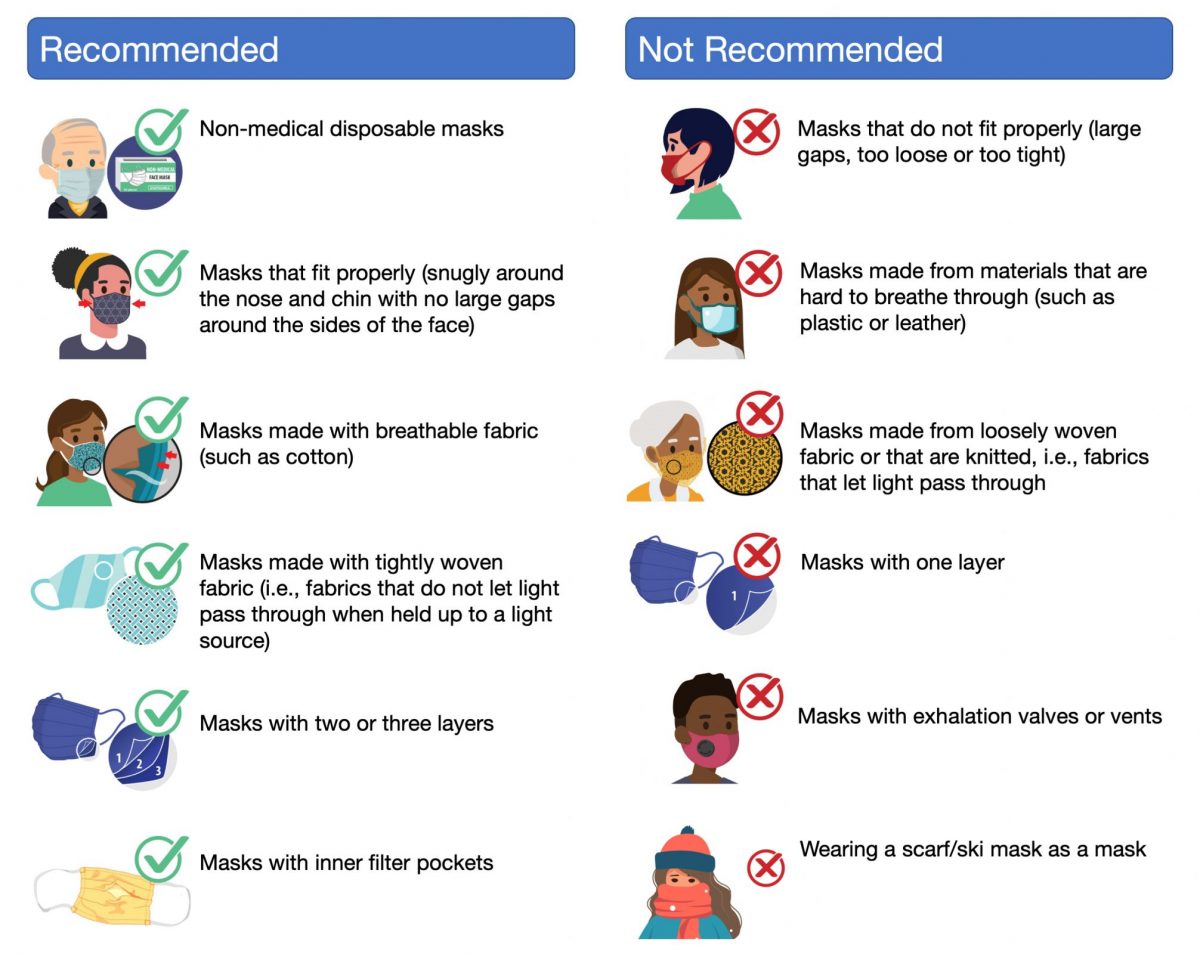
What are quarantine and self- isolation? What is the difference?
- “Quarantine” is a way to keep people who have been exposed to COVID-19 away from others until it’s clear that they do or do not have the virus. A close contact of someone with COVID-19 needs to stay at home for 14 days from their last contact with the infected person. If possible, people who are quarantining should pay particular attention to stay away from people who are at higher-risk for getting very sick from COVID-19.
- “Self-isolation” keeps people who have COVID-19 away from others who do not have COVID-19, even in their own home. If possible, try to have the person with COVID-19 stay in a specific “sick room” or an area away from other people or pets. They should also use a separate bathroom if one is available. A person with a positive COVID-19 test should self-isolate for at least 10 days from when symptoms first appeared (or from a positive test if they did not have symptoms) AND be at least 24 hours with no fever and improved symptoms.
Will I be notified if someone in my child’s school tests positive?
- If your child is considered to have been in close contact to someone who tests positive, you will be notified that they have been exposed via the contact tracing process. If there is a case in your school but your child has not been exposed, schools have different policies. Some will report cases publicly at the grade or school level, others will report cases at the district level. Ask your school how they plan to inform the school community about cases.
Vaccine
Should we get the COVID-19 vaccine when it’s available to us? What about kids?
- The CDC strongly recommends that everyone who is eligible get the COVID-19 vaccine. If you’re not sure if you’re eligible or if you have other questions, ask your health care provider.
- Currently, there are two vaccines available in the US made by two different companies. The Pfizer/BioNTech vaccine is approved for people 16 years and older. The Moderna vaccine is approved for people 18 years and older.
- Currently, there are no COVD-19 vaccines that are approved by the U.S. Food and Drug Administration (FDA) for anyone under the age of 16. The vaccine is being studied in children. It’s not clear when a vaccine will be approved children under age 16.
- For more information on the COVID-19 vaccine, visit:
- Children’s Hospital of Philadelphia vaccine resource page: https://www.chop.edu/centers-programs/vaccine-education-center/making-vaccines/prevent-covid
- The CDC COVID-19 information page: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/index.html
Other infection control strategies
What about ventilation in schools? What are schools doing to increase ventilation?
- Better ventilation can decrease the spread of COVID-19 by decreasing the number of small virus particles in the air. This is especially important in small or crowded spaces. Schools can improve ventilation by:
- Using outdoor space whenever possible
- Increasing circulation of outdoor air in indoor spaces
- Open windows when safe
- Open classroom doors when safe
- Install specialized filters or air purifiers
- MERV-13 filters are recommended for heating, ventilation, and air conditioning systems (HVAC)
- Portable air purifiers may be helpful, especially in buildings with systems that do not allow for MERV-13 filters
- Even with outdoor activities, or excellent indoor ventilation, masking, distancing, cohorting group of students together, and other safety measures should still be used.
How important is cleaning in schools?
- Cleaning is important, but probably not as critical as we once thought. The most important things for schools to clean are “high touch” surfaces–places and things that many kids touch (think pencil sharpeners, door handles, or shared materials in a classroom). These surfaces, along with bathrooms, are important to clean thoroughly on a regular basis. Since the virus must get to our faces to be infectious, cleaning hands regularly is just as important as cleaning surfaces.
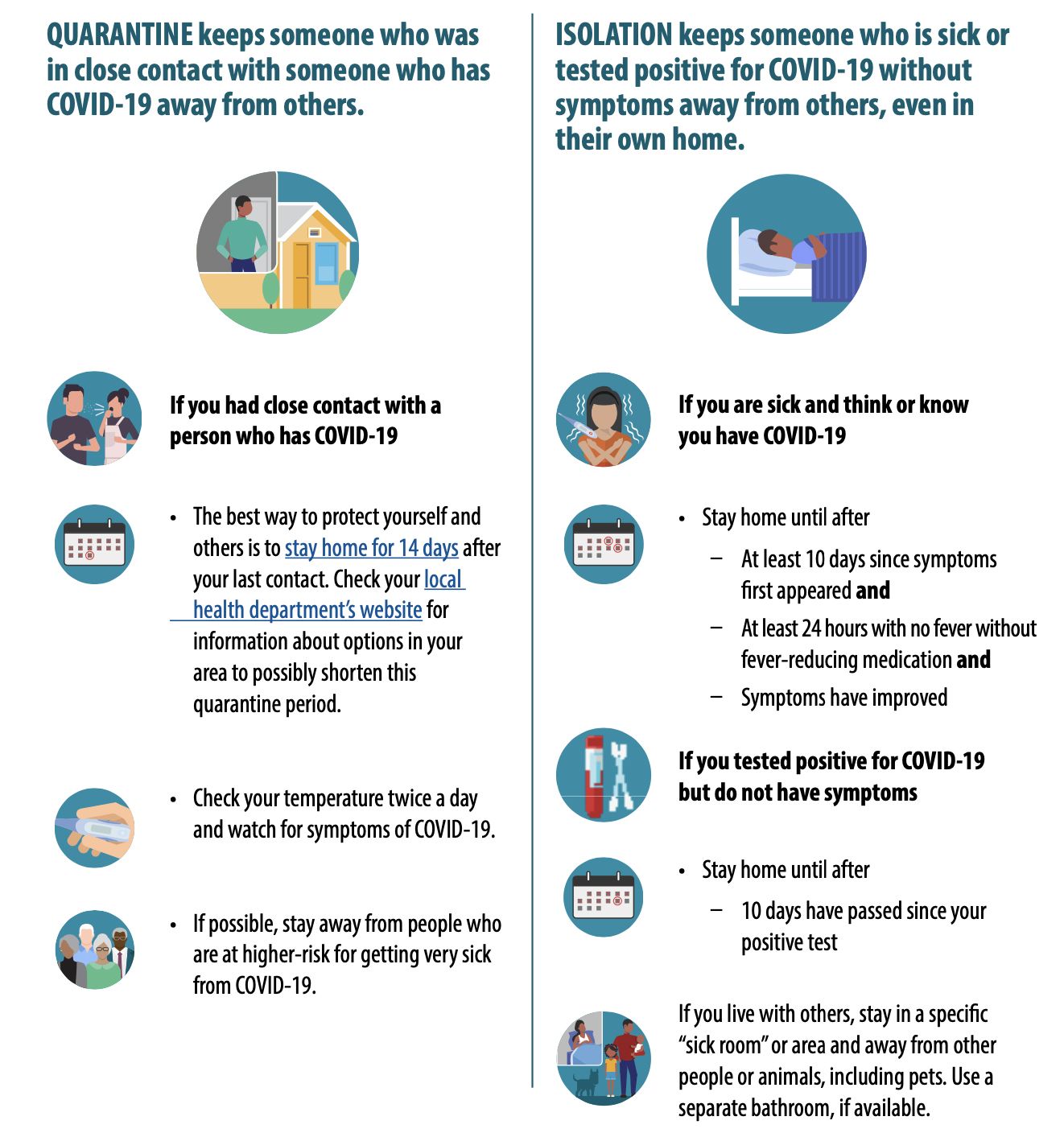
How does frequent hand washing help reduce the chances my child will get COVID-19?
- After sneezing, coughing, or touching our nose or mouth, we can get COVID virus on our hands. If we then touch another person or a shared object like a doorknob, the other person could get the virus on their hands. Frequent, proper hand washing removes the COVID virus and other germs from our hands so we can’t pass them around. Hands should be washed with soap and water for at least 20 seconds. Hand sanitizer with greater than 60% alcohol can also be used.
Does my child need to bathe or change clothes after in-person school?
- It is not necessary for your child to bathe or change clothes when they come home from school. The COVID-19 virus can survive on skin, hair, and clothes. However, people do not usually catch COVID-19 this way. They should remove their mask at the end of the day, and it should be washed before being worn again. Kids should be sure to wash their hands when they come home and often throughout the day. Wash for at least 20 seconds with soap and water or hand sanitizer with more than 60% alcohol.
General COVID-19 information
How is COVID-19 spread in schools?
COVID can be spread in three ways:
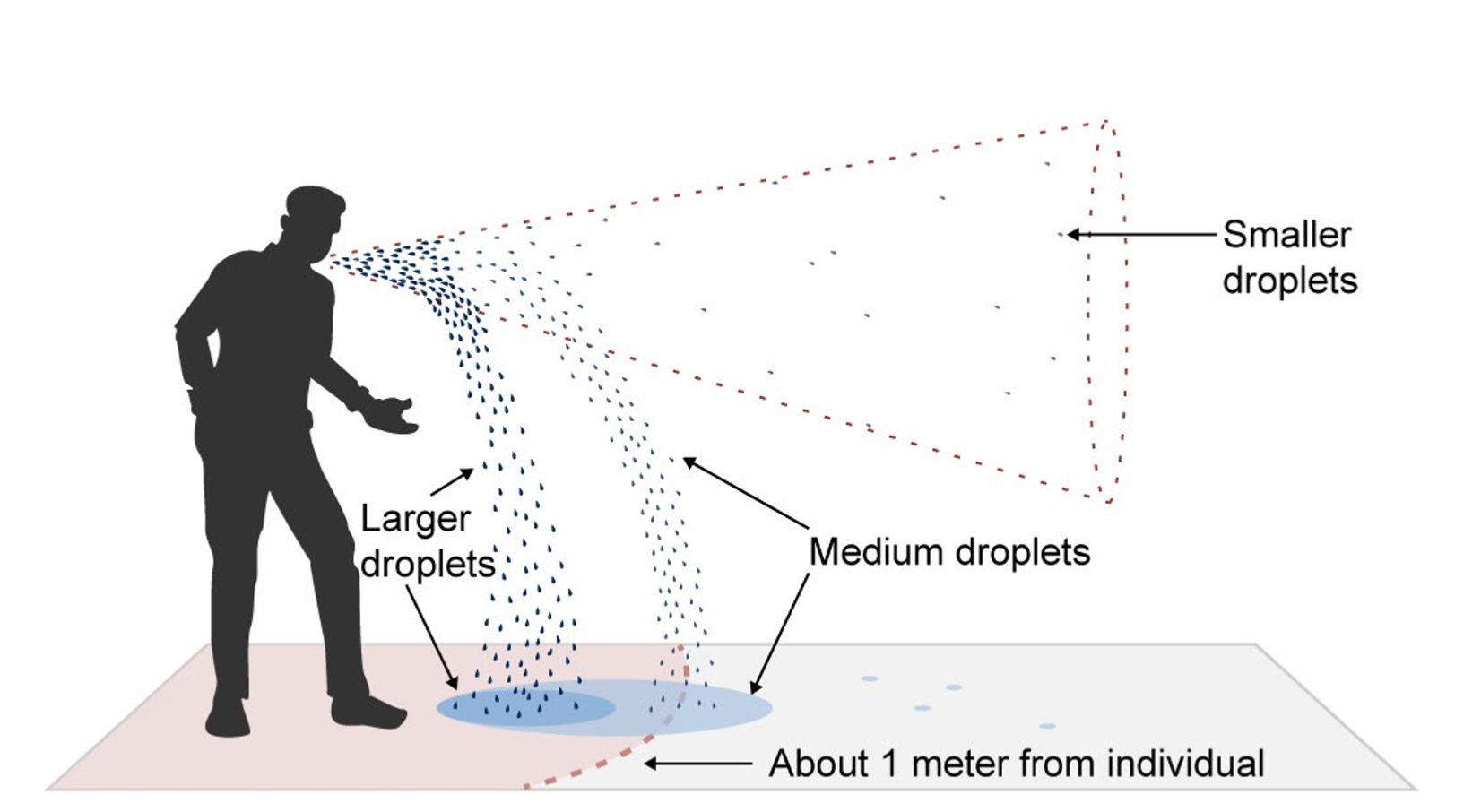
- From coming into close contact with someone who has COVID-19 (whether or not they have symptoms). Being in “close contact” usually means spending 15 minutes total within 6 feet of someone within 24 hours. Droplets containing the virus come out of the mouth and nose when people talk, shout, cough, sneeze, or sing. These droplets usually fall to the ground quickly within about 6 feet of the person (that’s why it’s recommended that people keep at least 6 feet apart). The farther away we are, the less likely these droplets will reach us. More distance= less risk.
- In the air. People with COVID-19 also produce very small droplets that may stay in the air for hours. These are usually diluted in the air unless someone is in a small, confined space (which is why good ventilation is important).
- From surfaces. The virus can be spread if a person touches a surface/object contaminated by respiratory droplets and then touches their face. The virus can live on surfaces from hours to days (depending on the surface)—as time passes, the amount of virus is usually not enough to be infectious. Catching COVID from paper or clothing, for example, is very unlikely. Washing hands frequently is important to make sure that if you touch your face, you’re not bringing the virus to your mouth or nose.
How can I minimize the chances that my family will get COVID-19?
- Research suggests that schools are not a major source of COVID-19 spread. Because there is still some risk of exposure in school, it is important to follow the school’s safety procedures carefully. It is also extra important to minimize risks at home and in the community.
- The most important ways to help decrease the chances that someone in your family will get COVID-19 are:
- Wear a mask whenever you are out in public or with people who are not members of your household.
- Keep at least 6ft of distance from people who are not members of your household.
- Avoid indoor gatherings, especially gatherings that involve people outside of your household.
- Stay home if you are sick or have been exposed to someone who is sick or who has COVID-19. Let the school know about your symptoms or your exposure and follow public health guidance about isolation.
- Get the COVID-19 vaccine when it is available to you.
Where can I get accurate information about COVID-19?
- For the latest information on COVID-19 guidance, symptoms and testing, vaccines, and COVID-19 transmission, visit the CDC here: https://www.cdc.gov/coronavirus/2019-ncov/index.html. For local information, visit your state or local health department website.
What about the new COVID-19 “variants”? What do those mean for COVID-19 risks in schools?
- Viruses are changing all the time. These changes lead to different variants of the COVID-19 virus. Some variants may be more or infectious than the “original” version of the virus. The same measures like masking, distancing, ventilation, hand washing, cohorting, and testing are still the way to prevent infection. The variants mean that schools will have to be very strict about their infection control measures since the virus that’s circulating in the local community may include versions that are more infectious.